NAUSAZY 4mg
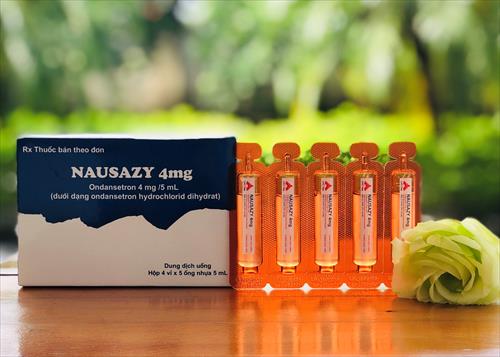
Active Element: Ondansetron (as Ondansetron hydrochloride dihydrate)
Dosage Form:
Composition
Ondansetron (as Ondansetron hydrochloride dihydrate) 4mg/5ml
Dosage Form
Liquid solution
Indication
The management of nausea and vomiting induced by cytotoxic chemotherapy and radiotherapy, and for the prevention of post-operative nausea and vomiting in adults.
Dosage Adminstration
Chemotherapy and radiotherapy induced nausea and vomiting.
Adults:
The emetogenic potential of cancer treatment varies according to the doses and combinations of chemotherapy and radiotherapy regimens used. The selection of dose regimen should be determined by the severity of the emetogenic challenge.
Emetogenic chemotherapy and radiotherapy: Nausazy can be given either by rectal, oral (tablets or syrup), intravenous or intramuscular administration.
For oral administration: 8 mg taken 1 to 2 hours before chemotherapy or radiation treatment, followed by 8 mg every 12 hours for a maximum of 5 days to protect against delayed or prolonged emesis.
For highly emetogenic chemotherapy: a single dose of up to 24 mg Nausazy taken with 12 mg oral dexamethasone sodium phosphate, 1 to 2 hours before chemotherapy, may be used.
To protect against delayed or prolonged emesis after the first 24 hours, oral or rectal treatment with Nausazy may be continued for up to 5 days after a course of treatment.
The recommended dose for oral administration is 8 mg to be taken twice daily.
Paediatric Population:
CINV in children aged ≥ 6 months and adolescents:
The dose for CINV can be calculated based on body surface area (BSA) or weight – see below. In paediatric clinical studies, ondansetron was given by IV infusion diluted in 25 to 50 mL of saline or other compatible infusion fluid and infused over not less than 15 minutes.
Weight-based dosing results in higher total daily doses compared to BSA-based dosing.
There are no data from controlled clinical trials on the use of Nausazy in the prevention of delayed or prolonged CINV. There are no data from controlled clinical trials on the use of Nausazy for radiotherapy-induced nausea and vomiting in children.
Dosing by BSA:
Nausazy should be administered immediately before chemotherapy as a single intravenous dose of 5 mg/m2. The single intravenous dose must not exceed 8 mg.
Oral dosing can commence 12 hours later and may be continued for up to 5 days (Table 1). The total dose over 24 hours (given as divided doses) must not exceed adult dose of 32 mg.
Table 1: BSA-based dosing for Chemotherapy - Children aged ≥6 months and adolescents
|
BSA |
Day 1 (a,b) |
Days 2-6(b) |
|
< 0.6 m2 |
5 mg/m2 IV plus 2 mg syrup after 12 hours |
2 mg syrup every 12 hours |
|
≥ 0.6 m2 to ≤ 1.2 m2 |
5 mg/m2 IV plus 4 mg syrup or tablet after 12 hours |
4 mg syrup or tablet every 12 hours |
|
> 1.2 m2 |
5 mg/m2 or 8 mg IV plus 8 mg syrup or tablet after 12 hours |
8 mg syrup or tablet every 12 hours |
a The intravenous dose must not exceed 8 mg.
b The total dose over 24 hours (given as divided doses) must not exceed adult dose of 32 mg
Dosing by bodyweight:
Weight-based dosing results in higher total daily doses compared to BSA-based dosing.
Nausazy should be administered immediately before chemotherapy as a single intravenous dose of 0.15 mg/kg. The intravenous dose must not exceed 8 mg.
Two further intravenous doses may be given in 4-hourly intervals.
Oral dosing can commence 12 hours later and may be continued for up to 5 days (Table 2). The total dose over 24 hours (given as divided doses) must not exceed adult dose of 32 mg.
Table 2: Weight-based dosing for Chemotherapy - Children aged ≥6 months and adolescents
|
Weight |
Day 1 (a,b) |
Days 2-6(b) |
|
≤ 10 kg |
Up to 3 doses of 0.15 mg/kg IV every 4 hours |
2 mg syrup every 12 hours |
|
> 10 kg |
Up to 3 doses of 0.15 mg/kg IV every 4 hours |
4 mg syrup or tablet every 12 hours |
a The intravenous dose must not exceed 8 mg.
b The total dose over 24 hours (given as divided doses) must not exceed adult dose of 32 mg.
Elderly:
No alteration of oral dose or frequency of administration is required.
Post operative nausea and vomiting (PONV).
Adults:
For the prevention of PONV: Nausazy can be administered orally or by intravenous or intramuscular injection.
For oral administration: 16 mg one hour prior to anaesthesia.
For the treatment of established PONV: Intravenous or intramuscular administration is recommended.
Paediatric population:
PONV in children aged ≥ 1 month and adolescents
Oral formulation:
No studies have been conducted on the use of orally administered ondansetron in the prevention or treatment of post-operative nausea and vomiting; slow IV injection (not less than 30 seconds) is recommended for this purpose.
Injection:
For prevention of PONV in paediatric patients having surgery performed under general anaesthesia, a single dose of ondansetron may be administered by slow intravenous injection (not less than 30 seconds) at a dose of 0.1 mg/kg up to a maximum of 4 mg either prior to, at or after induction of anaesthesia.
For the treatment of PONV after surgery in paediatric patients having surgery performed under general anaesthesia, a single dose of Nausazy may be administered by slow intravenous injection (not less than 30 seconds) at a dose of 0.1 mg/kg up to a maximum of 4 mg.
There are no data on the use of Nausazy in the treatment of PONV in children below 2 years of age.
Elderly:
There is limited experience in the use of Nausazy in the prevention and treatment of PONV in the elderly, however Nausazy is well tolerated in patients over 65 years receiving chemotherapy.
For both indications:
Patients with Renal impairment:
No alteration of daily dosage or frequency of dosing, or route of administration are required.
Patients with Hepatic impairment:
Clearance of Nausazy is significantly reduced and serum half life significantly prolonged in subjects with moderate or severe impairment of hepatic function. In such patients a total daily dose of 8 mg should not be exceeded.
Patients with poor Sparteine/Debrisoquine Metabolism:
The elimination half-life of ondansetron is not altered in subjects classified as poor metabolisers of sparteine and debrisoquine. Consequently in such patients repeat dosing will give drug exposure levels no different from those of the general population. No alteration of daily dosage or frequency of dosing is required.

